The full 411 on migraines
- Dr. Donald Littlewood
- Oct 29, 2020
- 9 min read
Are your migraines under control?
My name is Dr. Donald Littlewood & I am a chiropractor in downtown Toronto. I focus in treating headaches & neck pain as well as the LGBTQ+ community. Today, I am talking all things migraines -- what they are, how they are diagnosed, different treatment options & some at-home techniques you can use to stop them. So let’s get started.
Migraines suck. There is simply no nice way to put it. They suck.

But did you know that oftentimes those who think they have migraines actually have a different type of headache? In order to figure out why you are having a migraine, what could be triggering it, and how to treat it, we need to know if you are actually having a migraine.
Luckily, the International Headache Society lays out this information for us. In order to be officially diagnosed as a migraine, the following criteria have to be met:
You have to have a minimum of five “attacks”
Lasts 4-72h [or would if left untreated]
Two of the following four characteristics:
Unilateral location [only one side & it is usually the same side]
Pulsating quality
Moderate to severe in intensity
Aggravated by [or causes avoidance of] physical activity
At least one of the following:
Sensitivity to light and/or sound
Nausea and/or vomiting
Now if you are a migraineur, or know someone who is, you’ll likely have noticed that this criteria leaves something out. The infamous aura.
In order to be considered as a migraine with aura, all of the criteria above have to be met plus the addition of:
Fully reversible disturbances or changes in vision, sensory, speech, language, motor control, brainstem or retinal symptoms
At least two of the following characteristics:
At least one aura symptom comes on gradually over the course of 5+ minutes, and/or two or more symptoms occurring in succession
Each aura symptom lasts 5-60 minutes
At least one aura symptom is seen only on one side
Aura is accompanied, or followed within 60 minutes of, a headache
It’s a lot, I know. Which is why I am going to break.it.down for you.
A migraine is essentially a really bad one sided, pulsing headache. This headache can last for days and is made worse by physical activity. These headaches also cause sensitivity to light & sound as well as nausea and vomiting.
30% of people who have migraines will notice that they are preceded by an aura which is a sensory disturbance that warns you to some extent that a migraine is coming.
Now that we know what a migraine is, let’s talk how.

How does a migraine happen?
The short answer: we don’t fully know.
This is a classic answer. To be honest, doctors & scientists don’t really know the full ins and outs of what goes on in our bodies most of the time. The human body is a weird and wonderful thing and as much as we do know about it, there is even more we don’t know.
To an extent, the physiology of a migraine is one of those things. I do, however, want to share with you what we do know.
It is generally understood that a migraine occurs from a couple of different sources. So let’s talk about them.
Trigeminovascular pain pathway
Before you close this window, let me break this down for you. I’ll start with the basics.
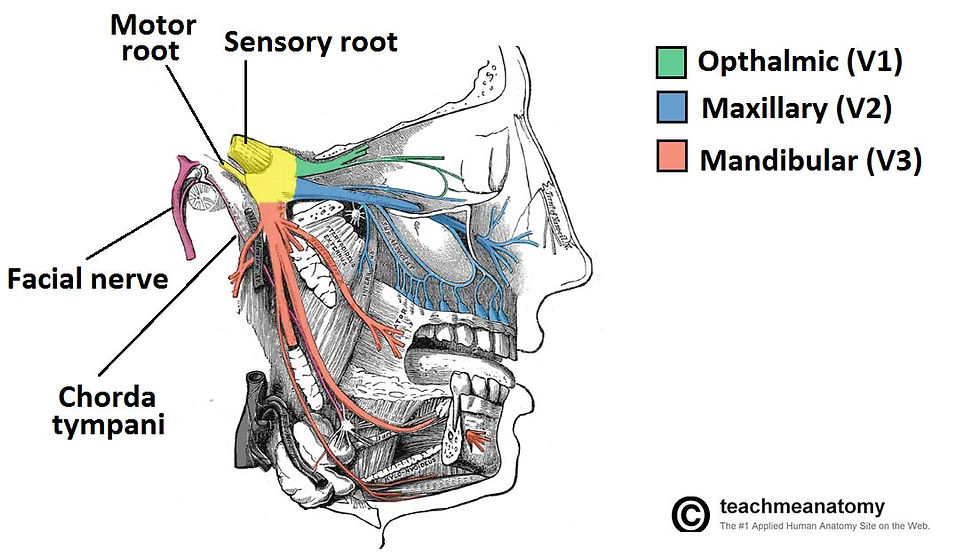
The trigeminal nerve [also known as cranial nerve V, or CN V] is one of the 12 cranial nerves of the body. These nerves emerge directly fr
om the bottom portion of the brain and control vision, smell, taste, chewing, facial expression, eye movements, swallowing, visceral, balance, and shoulder elevation. Of these 12 nerves, CN V is the most complex.
CN V has three parts [ophthalmic, maxillary & mandibular] and it is in charge of sensation to the face & mouth as well as motor control to the muscles of mastication - aka chewing. These three branches of CN V all converge on a structure called the trigeminal ganglion along with branches from the first and second cervical spinal nerves. This trigeminal ganglion takes all the sensory information these nerves receive, bundles it all up and sends it off through the brainstem to the thalamus for processing.
Why am I telling you this?
Well it comes down to the concept of referred pain.
All these nerves come together on the trigeminal ganglion to get packaged & sent to the brain. But when the information gets to the brain, it is unable to figure out exactly where you are having the issue. Your brain just knows that something is happening in the area.
Cortical spreading depression
CSD is a complex neurological process that may explain why some people get an aura with or before their headaches.
CSD involves local release of ATP [i.e., energy], glutamate [your body’s excitatory chemical], nitric oxide and other chemicals and ions. These molecules then head out to the surface of your brain where inflammation then happens. This inflammation is what is thought to cause the aura.
But what causes CSD? Well, just as with the trigeminovascular pathway, we don’t know. But there is an underlying thought that genetics play a significant role in aura production.
Migraine triggers
This is one of the most talked about aspects of migraine management. Most people find that their migraines are associated with an external trigger. These triggers can be food, environmental, scents, etc. Most people know what their triggers are, but I want to go through a few of the most common ones with you.

Nutrition/food
This is one of the most common triggers out there. Things like missing meals and inadequate hydration are common triggers, but there are also a lot of specific foods that should be considered when trying to nail down triggers.
Alcohol: the why behind this one is unknown [again, annoying, I know] but more than a quarter of those with migraines state that alcohol is a main trigger for them. Specifically red wine.
Biogenic amines: these are chemicals that our body makes on our own [like adrenaline], but also ones that we commonly ingest in our diets. Preliminary research has shown that ingesting biogenic amines might have an effect on migraines. Cheese, wine, cured meats, and fish are all high in biogenic amines.
Caffeine: caffeine can sometimes help a headache/migraine if you are already a caffeine consumer, but it can also cause migraines. Around 10% of those with migraines say that caffeine triggers them.
Hormones
There seems to be a correlation between menstruation and migraine development in two different ways. Migraines with an aura are more commonly seen with estrogen withdrawal or low estrogen and migraines without aura are more commonly seen when estrogen levels rise.
This is thought to be related to abnormal reactions between estrogen and neurotransmitters in your body such as serotonin & other endorphins.
Environment
The weather is a massive player in migraines with ~60% of migraine sufferers saying this is one of their main triggers. There is not really any data that supports this, but weather is a trigger that people cite no matter where they live. Some researchers think that this trigger may be an evolutionary mechanism to warn people of storms, but again, this has not been proven. There is definitely more research needed here.
Other things like perfumes, harsh lighting, sunlight & pollution are all commonly cited migraine triggers.
Psychological & physical stress
30-90% of the migraine population state that stress is a big trigger for them. Now I know that this is a huge range, but it is safe to say that migraineurs [and the rest of the population] should take stress reduction as a major way to decrease their pain.
And don’t you worry - I will get to stress reduction strategies in a bit!
Sleep & fatigue
Changes in your sleep pattern, time asleep, bed/wake time, etc. can all have profound effects on triggering migraines. 72% of those with migraines say that feeling tired/weak/weary is their main warning sign of a migraine. If you have migraines, prioritizing sleep & rest can make the world of difference.
Weekends
Huh? Weekends, really?
Yes. Two things come into play here:
Lifestyle: as a population, we tend to have less structure on weekends. Sleeping in, skipping breakfast, caffeine withdrawal & increased alcohol intake are all very common and very real migraine triggers.
Let down effect: the let down effect describes changes in our health that manifest after a stressful event. In the context of migraines, our weekdays are full of work and other stressors [time constraints, etc], but those daily stressors don’t happen as much on the weekend. When we all of a sudden go from very stressed to very relaxed the body’s heightened immune response stops and it can lead to us getting sick, or the resurgence of a migraine.
Non-pharmacological treatment of migraines
Here is what you have been waiting for - treatment!
But before I get there, I have to say: this portion is not meant to replace medical advice. It is for information only. If you are looking for individualized advice, please speak to a healthcare professional or reach out to me and I will help you the best I can.
Before I start treating a patient, we need to figure out goals. These are realistic & timely goals that put you in the forefront of your care. In migraine patients, we first see a decrease in either frequency or intensity. There is no way to tell which is going to happen first, but if frequency goes down first, intensity usually follows and vice versa.

Manual therapy
You might be thinking: if all of this migraine business is happening in my brain, then how can manual therapy be beneficial?
Well that is why the trigeminovascular pain pathway is so important.
Reminder: the trigeminal ganglion takes in sensory information from the first two cervical spinal nerves, otherwise known as C1 & C2. Once this ganglion takes the information & sends it for processing it can no longer determine exactly where the issue is located, only that it is coming from the trigeminal ganglion.
And what is innervated by these two nerves? Well a lot:
Muscles that depress the hyoid bone [which is suspended in the front of the neck] which is essential in swallowing and speech
Suboccipital muscles
Rectus capitis lateralis muscle
Sensation of the upper trapezius muscle as well as the skin of the neck and scalp [from the back of the skull all the way around to the front of the ear]
This is where the manual therapy comes in.
Because these muscles are so intimately related to the trigeminal ganglion, it stands to reason that treating them will help with migraines. Treating these muscles with soft tissue therapy helps relax them and also helps down-regulate the nervous system by releasing endorphins, your body’s happy chemicals.
The second portion of manual therapy lies in the adjustment. In migraines we often see joints that aren’t moving very well. These joints almost always correspond with the nerves I mentioned above and so I like to get in there and adjust joints that aren’t moving.
The extra movement provided by the adjustments helps with the decrease in range of motion and neck pain we commonly see. The effects are also thought to have an effect on the brain & the trigeminal ganglion because of their intimate relationship with the nerves.
Acupuncture
Acupuncture has been used for thousands of years to treat a whole host of different conditions from low back pain, to stress, to smoking cessation, and migraines.
Studies have shown that a combination of 10 standardized points as well as points that are individualized for the patient can reduce the frequency & intensity of a patient’s migraines over an 8 week treatment period.
In my practice, I have used acupuncture to treat migraines [and other headache diagnoses] with great success.
Nutriceuticals
These are defined as food or dietary supplements that provide a therapeutic benefit. They are commonly used by those who want to avoid the long term risks of taking prescription medication and research is showing that their efficacy is underestimated in the general population.
There are several different supplements that are commonly given to help with migraines, but I want to focus on one for this blog post, and that is magnesium.
Magnesium is an essential element in our body and it is involved in over 300 reactions making it one of the most abundant minerals. It is involved in muscle contraction/relaxation, energy production, glucose metabolism, nerve conduction and so much more. Including migraines.
Remember earlier in this blog post I talked about cortical spreading depression and how it is thought to be the physiological process behind an aura? Well as it turns out, a deficiency in magnesium can actually promote the occurrence of CSD as well as platelet forming and the narrowing of blood vessels. Having sufficient magnesium can also decrease that inflammation that occurs on the surface of the brain that we see in CSD.

Most of the evidence out there suggests that magnesium has its best effects when taken daily as a preventative measure and not as an in the moment relief measure. In fact, studies are showing that daily supplementation of magnesium glycinate can reduce migraine frequency by 41%!
Stress reduction
If you’ve been around these parts for a bit you’ll know that I am big on stress reduction. Chronic stress can wreak havoc on both our physical and mental wellbeing. I work on stress reduction a lot with my patients and it does truly make a difference in pain levels & quality of life.
One of the most effective ways to manage your stress is through deep, diaphragmatic breathing. Diaphragmatic breathing activates your parasympathetic nervous system which functions to calm you down and induce the body’s “rest & relax” phase.
Diaphragmatic breathing is simple. All you have to do is close your eyes and breathe through your abdomen instead of your chest.
Final thoughts
Migraines may not be the most common headache condition out there, but they have a big effect on the quality of life of the patient and those around them. If you are a migraine sufferer, it is so important that you find what works for you in terms of headache & symptom management.
If you are looking for more help, guidance & individualized care, please reach out and I would be happy to help, or find someone who can.

I thought that this was very very good. I have had migraines for a year and a sore neck, bad disc in back. This might help me with my migraines. My doctor gave me a pill for them I can’t afford $20 a pill crazy. I’m going to try theses things. Thanks very much